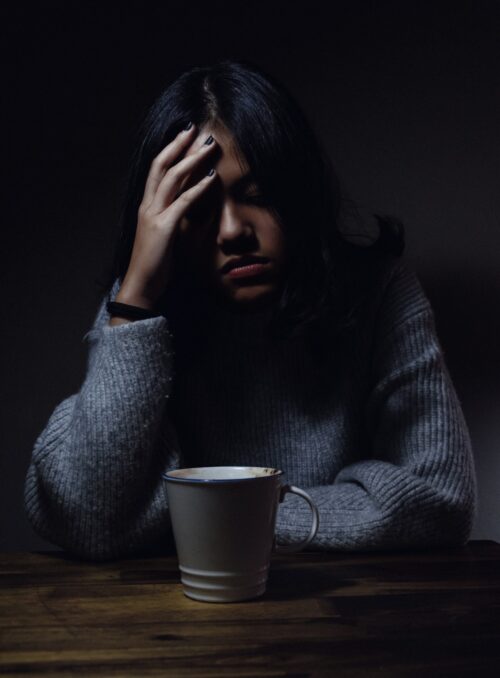
Psychotic depression, also known as major depressive disorder with psychotic features, is a severe mental health condition that combines the symptoms of depression with psychosis. People with this condition experience the debilitating effects of depression, such as profound sadness, hopelessness, and loss of interest in daily activities, along with psychotic symptoms like delusions and hallucinations. Psychotic depression is a complex and challenging condition to live with, as it affects a person’s thoughts, emotions, and perception of reality. Understanding the symptoms, causes, and treatment options for major depressive disorder is crucial for individuals living with this condition and their loved ones.
Psychotic symptoms in depression can manifest in different ways. Delusions, for example, are false beliefs that are not based on reality. Individuals with psychotic depression may hold beliefs that they are being persecuted, followed, or that they have committed unforgivable sins. Hallucinations, on the other hand, involve seeing, hearing, or feeling things that are not actually there. In psychotic depression, hallucinations are often auditory, with individuals hearing voices that criticize, insult, or command them.
Symptoms of psychotic depression
The symptoms of psychotic depression encompass both the characteristics of major depressive disorder and psychosis. These symptoms can vary in severity and duration, but they typically persist for at least two weeks. Some of the common symptoms of psychotic depression include:
- Persistent sadness and hopelessness: Individuals with psychotic depression experience an overwhelming feeling of sadness and hopelessness that persists throughout the day. They may lose interest in activities they once enjoyed and have difficulty finding pleasure in anything.
- Psychotic symptoms: Delusions and hallucinations are key features of psychotic depression. Individuals may have firmly-held false beliefs, such as being convinced that they are being monitored or controlled by external forces. They may also experience auditory hallucinations, hearing voices that are not there.
- Sleep disturbances: Insomnia or excessive sleepiness are common symptoms of psychotic depression. Some individuals may have trouble falling asleep or staying asleep, while others may struggle with excessive sleepiness and find it difficult to stay awake during the day.
- Changes in appetite: Psychotic depression can lead to significant changes in appetite. Some individuals may experience a loss of appetite and have no interest in food, while others may overeat and gain weight.
- Psychomotor agitation or retardation: Psychomotor symptoms involve noticeable changes in a person’s physical movements. In psychotic depression, individuals may either experience psychomotor agitation, where they feel restless and have an increased urge to move, or psychomotor retardation, where they feel slowed down and have difficulty moving.
Understanding the causes of major depressive disorder
The exact causes of psychotic depression are not fully understood. However, research suggests that it is likely a combination of genetic, biological, environmental, and psychological factors that contribute to the development of this condition. Some possible causes of psychotic depression and risk factors include:
- Genetic predisposition: Individuals with a family history of depression or psychosis may be more susceptible to developing psychotic depression. Certain genes and variations in gene expression have been associated with an increased risk.
- Brain chemistry: Imbalances in certain neurotransmitters, such as serotonin and dopamine, have been linked to depression and psychosis. Disruptions in the functioning of these chemicals can contribute to the development of psychotic depression.
- Stressful life events: Traumatic experiences, loss, or chronic stress can trigger the onset of psychotic depression. These events can disrupt the brain’s functioning and contribute to the development of depressive and psychotic symptoms.
- Medical conditions: Some medical conditions, such as Parkinson’s disease, multiple sclerosis, and certain types of cancer, have been associated with an increased risk of developing psychotic depression. Additionally, certain medications used to treat these conditions may also increase the risk.
- Substance abuse: Substance abuse, particularly the use of drugs like cocaine or amphetamines, can increase the risk of developing psychotic depression. These substances can disrupt brain chemistry and contribute to the onset of psychosis.
Diagnosing major depressive disorder
Diagnosing psychotic depression involves a comprehensive evaluation by a mental health professional. It typically includes a thorough assessment of the individual’s symptoms, medical history, and family history of mental health conditions. The diagnostic process may involve:
- Psychiatric evaluation: A psychiatrist or psychologist will conduct a detailed interview to gather information about the individual’s symptoms, their duration, and their impact on daily functioning. They may also inquire about any previous episodes of depression or psychosis.
- Physical examination: A physical examination may be conducted to rule out any underlying medical conditions that could be contributing to the symptoms. Blood tests may also be ordered to assess thyroid function and rule out other potential causes of depression.
- Diagnostic criteria: The mental health professional will compare the individual’s symptoms to the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). To be diagnosed with psychotic depression, an individual must meet specific criteria for both major depressive disorder and psychosis.
- Collateral information: In some cases, the mental health professional may seek input from family members or close friends to gain a better understanding of the individual’s symptoms and their impact on their life.
Once a diagnosis of psychotic depression is made, a comprehensive treatment plan can be developed to address the individual’s unique needs and symptoms.
Treatment options for major depressive disorder
Psychotic depression requires a combination of medical, psychological, and lifestyle interventions to effectively manage the symptoms and improve overall well-being. Treatment options may include medication, therapy and counseling, lifestyle changes, and support systems in Sydney, Melbourne, Brisbane, Perth, Adelaide and across Australia.
Medications for psychotic depression
Antidepressant medications are often prescribed to help alleviate the symptoms of depression in individuals with psychotic depression. Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) are commonly used. In some cases, antipsychotic medications may also be prescribed to target the psychotic symptoms. These medications help regulate brain chemistry and reduce the severity of symptoms.
Therapy and counseling for major depressive disorder
Various forms of therapy and counseling can be beneficial in treating psychotic depression. Cognitive-behavioral therapy (CBT) aims to identify and challenge negative thought patterns and behaviors associated with depression. It helps individuals develop healthier coping strategies and improve their overall mood. Psychodynamic therapy focuses on exploring the underlying causes of psychotic depression and addressing unresolved emotional conflicts.
Lifestyle changes to manage major depressive disorder
Making certain lifestyle changes can help individuals manage their symptoms and improve their overall well-being. Regular exercise, a balanced diet, and adequate sleep are essential for maintaining good mental health. Engaging in activities that bring joy and practicing stress-reducing techniques, such as meditation or yoga, can also be beneficial.
Support systems for individuals with major depressive disorder in Australia
Having a strong support system is crucial for individuals living with psychotic depression. In Sydney, Melbourne, Brisbane, Perth, Adelaide and across Australia, there are various support networks and organizations that provide assistance and resources for people with mental health conditions. These organizations offer helplines, support groups, and online forums where individuals can connect with others who may be experiencing similar challenges.
Coping strategies for dealing with major depressive disorder
In addition to professional treatment, individuals with psychotic depression can implement coping strategies to manage their symptoms on a daily basis. Some effective coping strategies include:
- Self-care: Engaging in activities that bring joy and relaxation, such as hobbies or spending time in nature.
- Social support: Seeking support from loved ones and joining support groups.
- Routine: Establishing a structured daily routine can provide a sense of stability and predictability.
- Stress management: Learning stress management techniques, such as deep breathing exercises or mindfulness, can help reduce symptoms.
Conclusion
Psychotic depression is a complex mental health condition that combines the symptoms of depression with psychosis. It can have a profound impact on a person’s thoughts, emotions, and perception of reality. Understanding the symptoms, causes, and treatment options for major depressive disorder is crucial for individuals living with this condition and their loved ones. By seeking professional help, implementing effective coping strategies, and accessing support systems, individuals with psychotic depression can lead fulfilling lives and manage their symptoms effectively. If you are interested in standard mental health first aid training, contact WHS and Training Compliance Solutions for more information.
Note: This article is for informational purposes only and should not be considered as a substitute for professional medical advice. Always consult with a qualified healthcare professional for an accurate diagnosis and appropriate treatment options.