Obsessive-Compulsive Disorder (OCD) is a mental health condition that affects millions of people worldwide. It is characterized by intrusive thoughts and repetitive behaviors that can significantly impact a person’s daily life. In this article, we will delve into the intricacies of OCD, exploring its symptoms, causes, diagnosis, and treatment options. By shedding light on this often misunderstood disorder, we aim to promote understanding, empathy, and destigmatization.
Understanding Obsessive-Compulsive Disorder (OCD)
Obsessive-Compulsive Disorder is a chronic mental health condition that manifests in two main components: obsessions and compulsions. Obsessions are recurring and intrusive thoughts, urges, or mental images that cause distress and anxiety. Compulsions, on the other hand, are repetitive behaviors or mental acts performed in response to the obsessions, aimed at reducing anxiety or preventing a feared outcome.
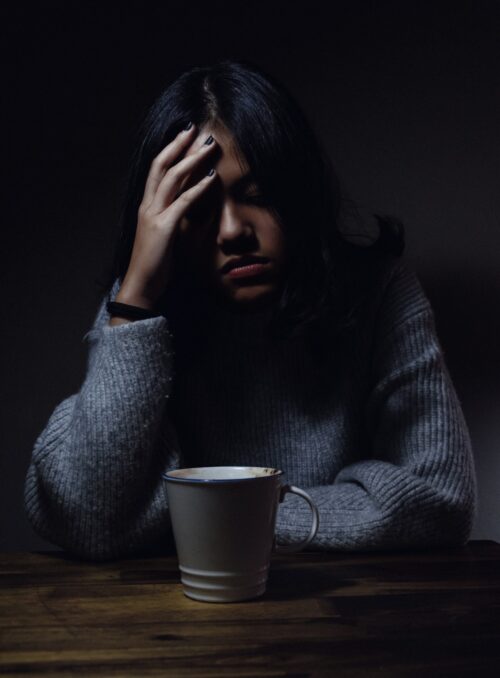
Individuals with OCD often find themselves trapped in a vicious cycle of obsessions and compulsions. The obsessions create intense anxiety, and to alleviate this anxiety, they feel compelled to engage in repetitive behaviors. These compulsions may temporarily relieve the anxiety, but the relief is short-lived, leading to a never-ending cycle of obsessions and compulsions.
Common symptoms of OCD
OCD can manifest in a wide range of symptoms, each unique to the individual. Some common obsessions include fear of contamination, aggressive or taboo thoughts, need for symmetry or exactness, and excessive doubts. Compulsions can take the form of excessive handwashing, repetitive checking, counting, arranging objects in a specific order, or seeking reassurance from others.
It is important to note that not all repetitive behaviors or intrusive thoughts are indicative of OCD. The key distinction lies in the severity and impact on daily functioning. If these symptoms significantly interfere with a person’s life, relationships, and overall well-being, a diagnosis of OCD may be warranted.
Causes and risk factors for developing OCD
The exact cause of OCD remains unknown, but research suggests that a combination of genetic, biological, environmental, and psychological factors contribute to its development. There is evidence to suggest that OCD can run in families, indicating a genetic predisposition. Additionally, imbalances in certain neurotransmitters, such as serotonin, have been linked to the disorder.
Environmental factors, such as childhood trauma or stressful life events, can also play a role in triggering OCD symptoms. Psychological factors, including perfectionism and a tendency towards excessive worrying, may increase the likelihood of developing the disorder.
How is OCD diagnosed?
Diagnosing OCD involves a thorough evaluation of symptoms, medical history, and a psychological assessment. A qualified mental health professional, such as a psychiatrist or psychologist, will conduct the assessment. They will use standardized criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to determine whether the symptoms meet the criteria for a diagnosis of OCD.
It is essential to consult a professional for an accurate diagnosis, as OCD can be mistaken for other mental health conditions with similar symptoms. Once diagnosed, a treatment plan can be tailored to the individual’s specific needs.
Treatment options for OCD
While there is no cure for OCD, there are effective treatments available to manage the symptoms and improve the quality of life for individuals with the disorder. The two main treatment options for OCD are cognitive-behavioral therapy (CBT) and medication.
Cognitive-behavioral therapy for OCD
CBT is a type of psychotherapy that focuses on identifying and challenging the negative thought patterns and beliefs that drive obsessions and compulsions. It aims to modify the distorted thinking patterns and help individuals develop healthier coping mechanisms. Exposure and response prevention (ERP), a specific form of CBT, is often used in the treatment of OCD. It involves gradually exposing individuals to their fears or triggers and preventing the associated compulsive behaviors.
Medications for OCD
In some cases, medication may be prescribed in conjunction with therapy to manage OCD symptoms. Selective serotonin reuptake inhibitors (SSRIs), a type of antidepressant, are commonly used to treat OCD. These medications help regulate serotonin levels in the brain, which can reduce anxiety and obsessions. Other medications, such as tricyclic antidepressants or antipsychotics, may be prescribed if SSRIs are ineffective.
Lifestyle changes to manage OCD symptoms
In addition to therapy and medication, certain lifestyle changes can help individuals manage their OCD symptoms effectively. These include maintaining a structured routine, practicing stress-reducing techniques such as mindfulness and relaxation exercises, and engaging in regular physical activity. It is also important to establish a strong support system and surround oneself with understanding and empathetic individuals.
Support groups and resources for individuals with OCD
Living with OCD can be challenging, but support groups and resources can provide much-needed assistance and understanding. There are numerous organizations, both online and offline, that offer support, information, and guidance for individuals with OCD and their loved ones. Support groups allow individuals to connect with others who share similar experiences, providing a sense of validation, comfort, and a platform to share coping strategies.
Living with OCD: Tips for managing daily life
Managing daily life with OCD requires patience, self-compassion, and the implementation of coping strategies. It is crucial to create a structured routine, prioritize self-care, and practice stress management techniques. Engaging in activities that bring joy and fulfillment can also help distract from obsessive thoughts. Open communication with loved ones about the condition and its impact is essential for receiving support and understanding.
Helping a loved one with OCD
If someone you care about is living with OCD, it is important to approach the situation with empathy and understanding. Educate yourself about the disorder, listen without judgment, and offer support without enabling their compulsions. Encouraging them to seek professional help and providing reassurance can make a significant difference in their journey towards recovery.
The importance of destigmatizing
Destigmatizing OCD is crucial for creating a supportive and inclusive society. It is essential to challenge misconceptions and stereotypes surrounding the disorder, promoting empathy and understanding. By raising awareness, educating others, and fostering open dialogue, we can create an environment where individuals with OCD feel accepted and supported.
Conclusion
Obsessive-Compulsive Disorder is a complex mental health condition that affects millions of people worldwide. By understanding its symptoms, causes, and treatment options, we can demystify and promote a greater sense of empathy and support for individuals living with the disorder. Through therapy, medication, lifestyle changes, and a strong support system, individuals with OCD can manage their symptoms effectively and lead fulfilling lives. Let us work together to destigmatize and create a more inclusive society for all.
Access Mental Health Awareness Books from Amazon: Mental Health Books